TAG:
Bundled payment
Bundled payment, also known as episode-based payment, episode payment, episode-of-care payment, case rate, evidence-based case rate, global bundled payment, global payment, package pricing, or packaged pricing, is defined as the reimbursement of health care providers (such as hospitals and physicians) “on the basis of expected costs for clinically-defined episodes of care.” It has been described as “a middle ground” between fee-for-service reimbursement (in which providers are paid for each service rendered to a patient) and capitation (in which providers are paid a “lump sum” per patient regardless of how many services the patient receives).
Advocates of bundled payments note that unlike fee-for-service, bundled payment discourages unnecessary care, encourages coordination across providers, and potentially improves quality. Unlike capitation, bundled payment does not penalize providers for caring for sicker patients. Bundling payment provides additional advantages to providers and patients alike, through removing inefficiency and redundancy from patient-care protocols; e.g. duplicate testing, delivering unnecessary care, and failing to adequately provide postoperative care.
This method of payment is also said to provide transparency for consumers by fixing pricing and publishing cost and outcomes data. Patients would be able to choose a provider based on a comparison of real data, not word of mouth. Bundled payments may also encourage economies of scale – especially if providers agree to use a single product or type of medical supply – as hospitals or integrated health systems can often negotiate better prices if they purchase supplies in bulk.
On the other hand, the scientific evidence in support of it has been described as “scant.” It does not discourage unnecessary episodes of care; for example, physicians might hospitalize some patients unnecessarily.
Providers may seek to maximize profit by avoiding patients for whom reimbursement may be inadequate (e.g., patients who do not take their drugs as prescribed), by overstating the severity of an illness, by giving the lowest level of service possible, by not diagnosing complications of a treatment before the end date of the bundled payment, or by delaying post-hospital care until after the end date of the bundled payment.
Meanwhile, early evidence indicates that Medicare’s bundled-payment pilot, the Bundled Payment Care Initiative, has helped participating providers improve the quality of care while better managing healthcare costs. Should more detailed findings confirm these outcomes, Medicare could decide to expand the range of clinical services it wants covered by a bundled-payment arrangement.
Lab Industry to Confront Major Issues during 2015
By Robert Michel | From the Volume XXII No. 1 – January 5, 2015 Issue
CEO SUMMARY: Will 2015 turn out to be a watershed year for the clinical laboratory industry? Not only are two federal agencies pushing forward with initiatives that will touch nearly every medical lab in the United States in the next 12 months, but other equally powerful trends c…
Doctors at Johns Hopkins Improve Lab Test Utilization
By Joseph Burns | From the Volume XXI No. 14 – October 13, 2014 Issue
CEO SUMMARY: Efforts to help physicians improve their utilization of clinical lab tests paid big dividends at the Johns Hopkins Bayview Medical Center in Baltimore, Maryland. Working collaboratively, physicians and the clinical lab team identified overused or needless cardiac biomarker te…
To Be Paid More, Labs Must Deliver More Value
By R. Lewis Dark | From the Volume XXI No. 13 – September 22, 2014 Issue
GETTING PAID FOR LAB TESTS IS BECOMING A MORE URGENT PRIORITY for both clinical laboratories and anatomic pathology groups this year. Multiple factors are responsible for lengthening the collection cycle and reducing overall reimbursement for lab testing. Clients of THE DARK REPORT have followed our…
Pathologists Face Unsettling Times
By R. Lewis Dark | From the Volume XXI NO. 6 – April 28, 2014 Issue
THESE ARE UNSETTLING TIMES FOR PATHOLOGISTS, particularly those who practice in a private pathology group that serves one or more community hospitals. Blame it on healthcare’s unfolding transformation and the new aggressiveness of payers to cut the prices they pay for anatomic pathology services. …
Better Data Needed to Support Pathologists as Consultants
By Joseph Burns | From the Volume XXI No. 4 – March 17, 2014 Issue
MULTIPLE TRENDS ARE UNFOLDING that mutually reinforce the need for pathologists and PhDs to be experts and consultants in how physicians order and follow up on molecular diagnostics assays and genetic tests. “Healthcare in the United States is approaching a tipping point that can greatly favor pat…
Labs, Path Groups Face Major Financial Issues
By Robert Michel | From the Volume XXI No. 3 – February 24, 2014 Issue
CEO SUMMARY: Are clinical labs and pathology groups ready for the end of fee-for-service reimbursement? That’s just one important question that will be answered at the upcoming Executive War College on Lab and Pathology Management that will take place in New Orleans on April 29-30. The …
Medicare OPPS Rule Has Pitfalls for Labs
By Joseph Burns | From the Volume XXI No. 2 – February 3, 2014 Issue
CEO SUMMARY: On January 1, the new Medicare rule for requiring bundled or packaged reimbursement for certain services covered by the hospital Outpatient Prospective Payment System (OPPS) became effective. Just four days earlier (on December 27), Medicare officials issued instructions on h…
ACLA, CAP Comment on Final 2014 Medicare Rules
By Joseph Burns | From the Volume XX, No. 16 – December 2, 2013 Issue
CEO SUMMARY: On November 27, as the nation prepared for the Thanksgiving holiday, the federal Centers for Medicare & Medicaid Services (CMS) announced the long-awaited final rules for 2014. Early analysis of the 1,300 pages of rules CMS released indicates that the agency moderated one…
Laboratory Offers Early Lessons in Positioning for Success with ACOs
By Joseph Burns | From the Volume XX No. 10 – July 29, 2013 Issue
CEO SUMMARY: Accountable care organizations (ACOs) are already leading the shift from fee-for-service reimbursement to population payment. ACOs are leading healthcare’s evolution to preventive care, wellness, and better management of patients with chronic disease. This evolution will re…
Executive War College Sessions Center Upon Three Trends
By Joseph Burns | From the Volume XX No. 6 – May 6, 2013 Issue
CEO SUMMARY: There was an interesting blend of anxiety and optimism as a record crowd gathered in New Orleans last week for the 18th annual Executive War College on Laboratory and Pathology Management. The anxiety was rooted in the shrinking prices paid by payers for lab testing services….
CURRENT ISSUE
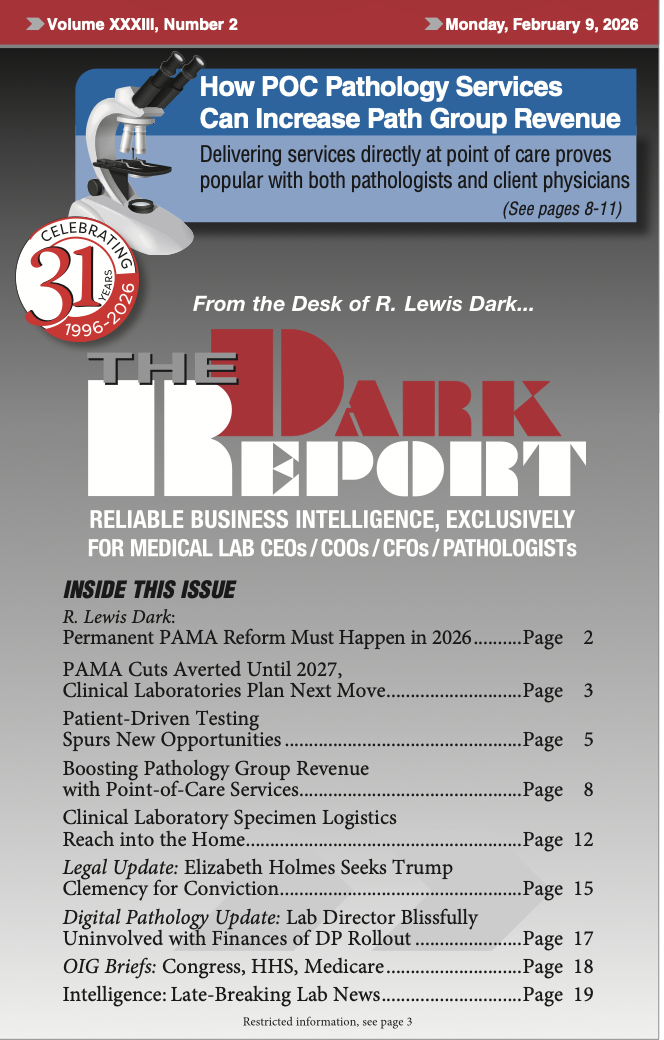
Volume XXXIII, No. 2 – February 9, 2026
Congress has once again delayed cuts to test reimbursement rates under PAMA, this time until Jan. 1, 2027. Laboratory professionals are urged to lobby Congress to pass the RESULTS act to solve the PAMA cuts problem permanently. Also, patient-driven testing is spurring new opportunities.
See the full table of contentsHow Much Laboratory Business Intelligence Have You Missed?
Lab leaders rely on THE DARK REPORT for actionable intelligence on important developments in the business of laboratory testing. Maximize the money you make-and the money you keep! Best of all, it is released every three weeks!
Sign up for TDR Insider
Join the Dark Intelligence Group FREE and get TDR Insider FREE!
Never miss a single update on the issues that matter to you and your business.
Topics
- Anatomic Pathology
- Clinical Chemistry
- Clinical Laboratory
- Clinical Laboratory Trends
- Digital Pathology
- Genetic Testing
- In Vitro Diagnostics
- IVD/Lab Informatics
- Lab Intelligence
- Lab Marketplace
- Lab Risk & Compliance
- Laboratory Automation
- Laboratory Billing
- Laboratory Compliance
- Laboratory Equipment
- Laboratory Information Systems
- Laboratory Management
- Lean Six Sigma
- Managed Care Contracts
- Molecular Diagnostics
- Pathology Trends
- People
- Uncategorized

