CEO SUMMARY: Forget CHINs from the 1990s and RHIOs from this decade. The future of regional health data repositories may turn out to be a patient-controlled model, often called a “Health Record Bank” (HRB). Here is the lab industry’s first look at this nascent movement. HRBs are under development in Louisville, Kentucky, the State of …
Health Record Databanks Are Different Than RHIOs Read More »
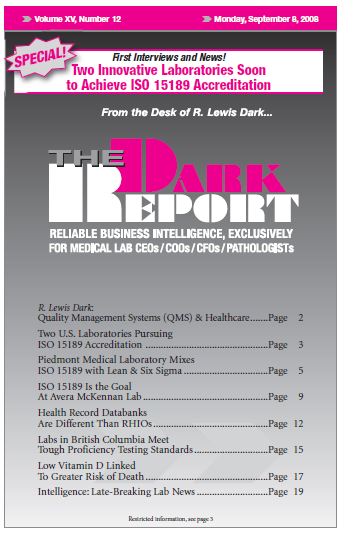
To access this post, you must purchase The Dark Report.