CEO SUMMARY: A new report in the Archives of Internal Medicine is likely to further spur demand for vitamin D testing. Already, labs are dealing with a dramatic increase in testing for vitamin D deficiency, with test volumes more than doubling in the past 12 months. This new research is considered the most definitive to …
Low Vitamin D Linked To Greater Risk of Death Read More »
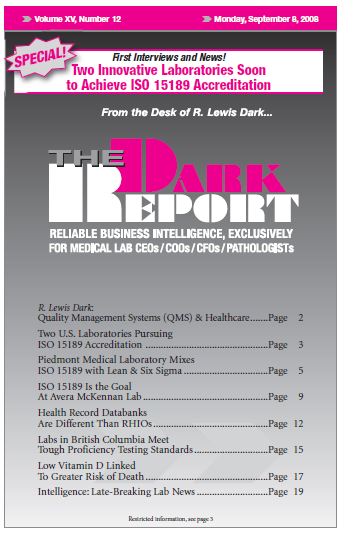
To access this post, you must purchase The Dark Report.