CEO SUMMARY: It must be rewarding for federal rulemakers at the Centers for Medicare and Medicaid Services and the Office of the Inspector General to hear that attorneys representing clinical labs and pathology groups consider the new final rules for the Stark Law and the Anti-Kickback Statute to be helpful for clarifying how labs and …
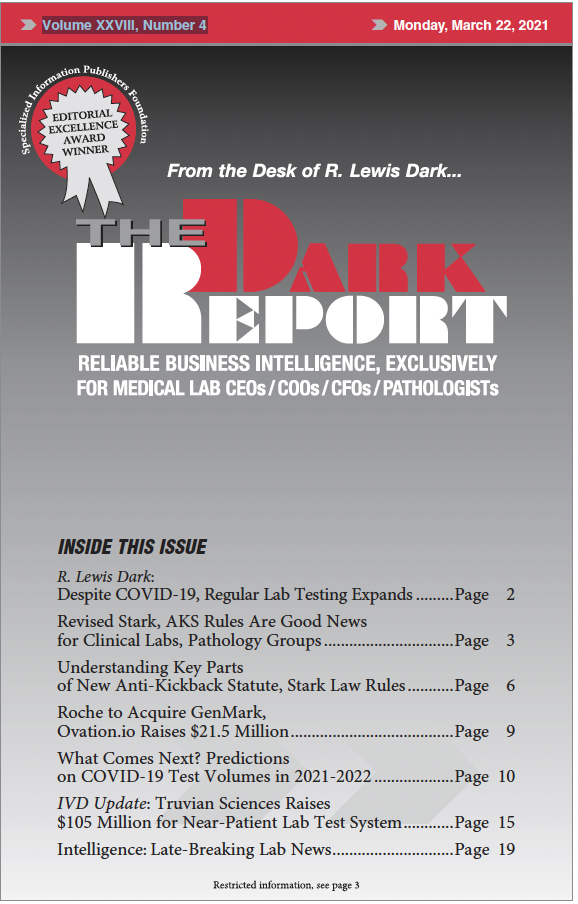
Revised Stark and AKS Rules Are Good News for Labs Read More »
To access this post, you must purchase The Dark Report.