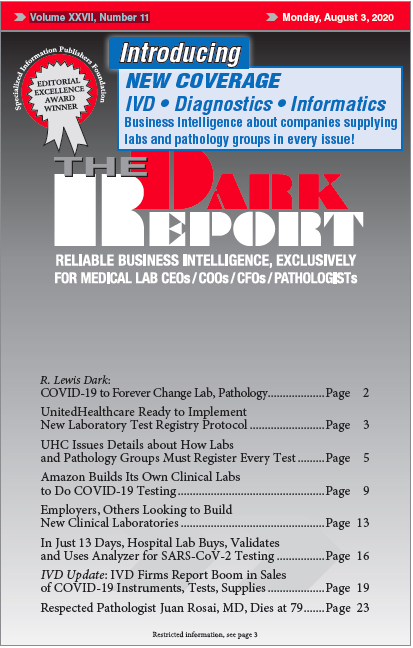
CEO SUMMARY: As of January 1, UnitedHealthcare will require all clinical laboratories and anatomic pathology groups to register every type of test before labs can bill for those tests. Not only is the COVID-19 pandemic disrupting normal activity, but the administrative burden UHC is imposing will be substantial for all of UHC’s in-network labs and pathology groups, as well as for …
UHC Issues Details about How Labs Register Tests Read More »
To access this post, you must purchase The Dark Report.