CEO SUMMARY: Cigna was the first national health insurer to require independent board-certified genetic counseling before approving coverage for certain genetic tests. Since launching this program in September 2013, the insurer has seen a 450% increase in genetic counseling for Cigna members. Such counseling has helped to reduce utilization of genetic testing because informed patients understand that a genetic test might not …
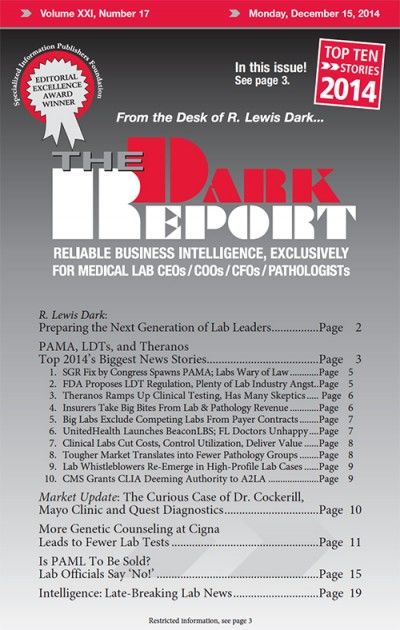
More Genetic Counseling Leads to Fewer Lab Tests Read More »
To access this post, you must purchase The Dark Report.