CEO SUMMARY: Several genetic testing companies have noticed that some of the nation’s Medicare Administrative Contractors (MAC) pay about $2,000 for test claims billed with CPT code 81408. From 2018 through and 2019, the number of 81408 claims rose dramatically at just two of these federal contractors: Novitas Solutions and First Coast Service Options. This …
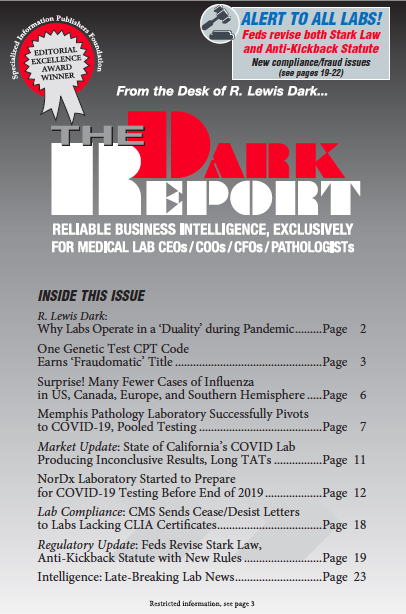
One Genetic Test CPT Code Earns ‘Fraudomatic’ Title Read More »
To access this post, you must purchase The Dark Report.