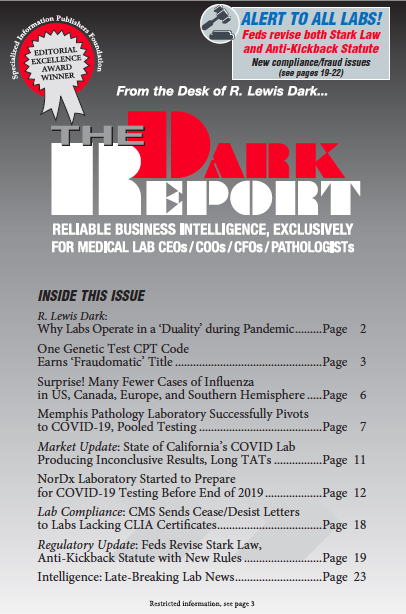
CEO SUMMARY: It is essential that all clinical laboratories and anatomic pathology groups understand major changes in two new federal rules that take effect next month. Revisions to the Physician Self-Referral Law (also known as the Stark Law) and the Anti-Kickback Statue will have wide-ranging effects on how clinical labs engage in value-based and care-coordination …
Feds Revise Stark Law, Anti-Kickback Statute Read More »
To access this post, you must purchase The Dark Report.