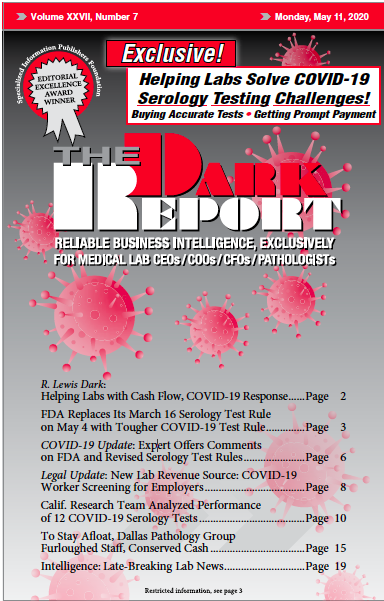
CEO SUMMARY: In the rush to allow companies and clinical laboratories to develop, validate, and bring to market serological tests for COVID-19, the federal Food and Drug Administration issued rules on March 16 that eased its requirements for these new assays. Because of the lack of oversight under the March 16 rules, the market was flooded with tests, including some …
FDA Replaces March 16 Serology COVID-19 Rules Read More »
To access this post, you must purchase The Dark Report.