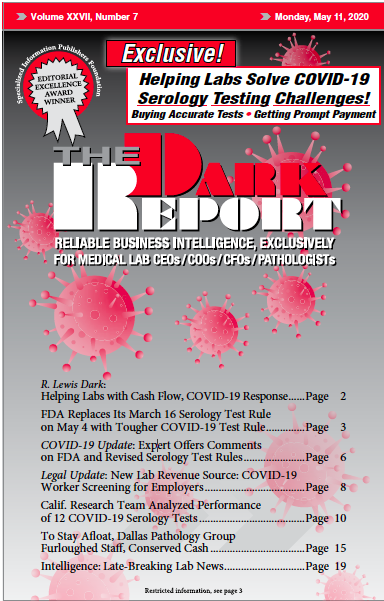
CLINICAL LABORATORY DIRECTORS are asking what caused the federal Food and Drug Administration (FDA) to issue a highly questionable policy in March to allow serological tests for SARS-CoV-2 and then change that policy seven weeks later. Under a policy the agency issued March 16, the FDA granted what it called “regulatory flexibility for developers offering such tests without FDA review and without an emergency use …
Expert Offers Comments on FDA and Revised Serology Test Rules Read More »
To access this post, you must purchase The Dark Report.