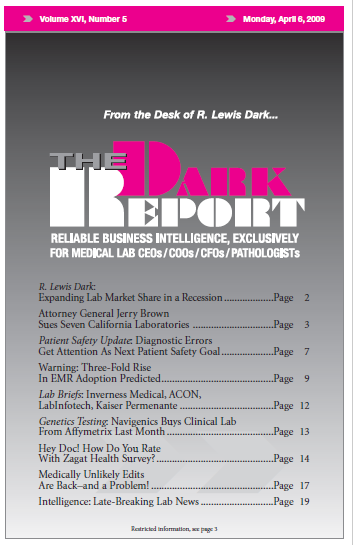
PHYSICIAN LEADERS IN PATIENT SAFETY are turning up the heat on doctors to reduce the incidence of diagnostic errors. This is a topic few dared to openly discuss until recently. It is directly linked to Medicare and private payer efforts to crack down on medical errors. This development has profound consequences for pathologists and laboratory …
Diagnostic Errors Get Attention As Next Patient Safety Goal Read More »
To access this post, you must purchase The Dark Report.