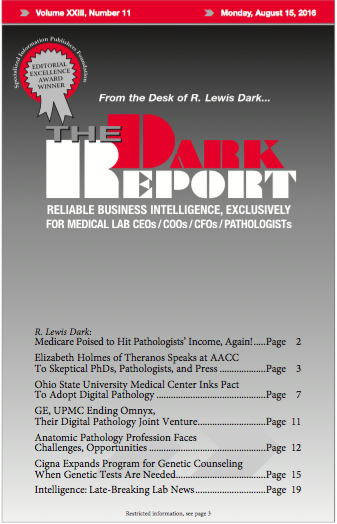
CEO SUMMARY: For 10 years, three primary trends have reshaped the anatomic pathology profession. They are declining reimbursement, competition from physicians establishing in-office pathology labs, and a host of new government laws and regulations. More changes are coming, predicts one business expert in pathology. Those changes involve new Medicare payment models, along with opportunities for …
Anatomic Pathology Profession Faces Challenges, Opportunities Read More »
To access this post, you must purchase The Dark Report.