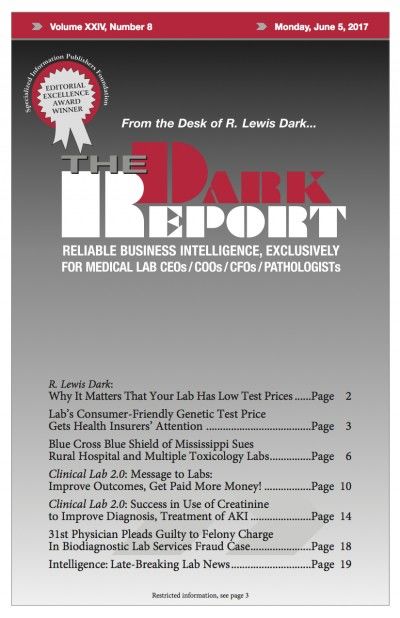
This is an excerpt from a 1,485-word article in the June 5, 2017 issue of THE DARK REPORT. The complete article is available for a limited time to all readers, and available at all times to paid members of the Dark Intelligence Group. CEO SUMMARY: At a time when most molecular and genetic testing companies …
California company shows labs the way with low genetic testing cost Read More »
To access this post, you must purchase The Dark Report.