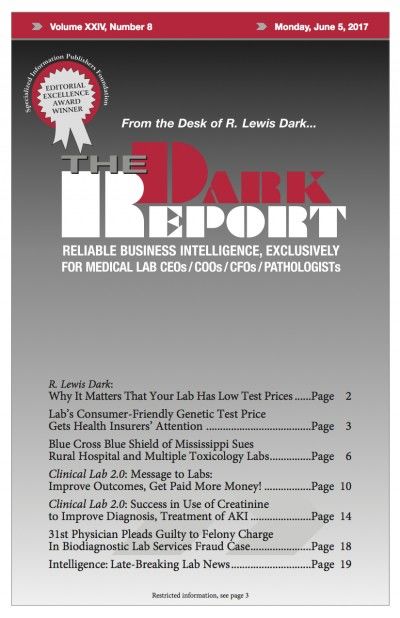
CEO SUMMARY: At a time when most molecular and genetic testing companies are struggling to gain coverage for their tests, this Silicon Valley-based lab company has become an in-network lab provider for a number of health insurers—including three of the nation’s largest payers. It did this by establishing a patient-friendly price of $249 for its …
Lab’s Low Gene Test Price Gets Insurers’ Attention Read More »
To access this post, you must purchase The Dark Report.