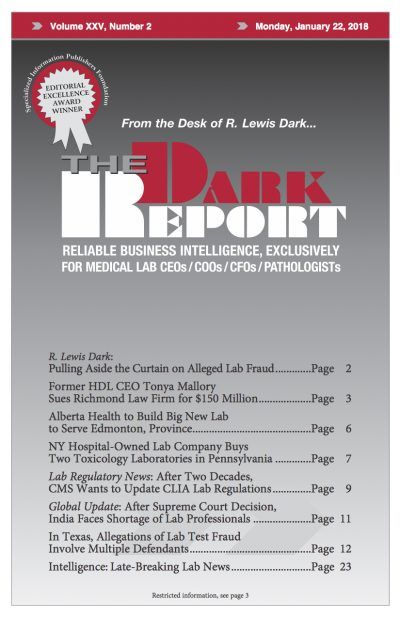
This is an excerpt from a 5,000-word article in the January 22, 2018, issue of THE DARK REPORT. The complete article is available for a limited time to all readers, and available at all times to paid members of the Dark Intelligence Group. CEO SUMMARY: UnitedHealth made national news when it filed a $100 million lawsuit […]
To access this post, you must purchase The Dark Report.