TAG:
Electronic health record (EHR)
An electronic health record (EHR) is a digital version of a patient’s paper chart. EHRs are real-time, patient-centered digital medical records that make information available instantly and securely to authorized users. While an EHR does contain the medical and treatment histories of patients, an EHR system is built to go beyond standard clinical data collected in a provider’s office and can be inclusive of a broader view of a patient’s care.
EHRs can:
- Contain a patient’s medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory and test results
- Allow access to evidence-based tools that providers can use to make decisions about a patient’s care
- Automate and streamline provider workflow
One of the key features of an EHR is that health information can be created and managed by authorized providers in a digital format capable of being shared with other providers across more than one health care organization. EHRs are built to share information with other health care providers and organizations – such as clinical laboratories, specialists, medical imaging centers, pharmacies, emergency facilities, and school and workplace clinics – so they contain information from all clinicians involved in a patient’s care.
According to HealthIT.gov, “A greater and more seamless flow of information within a digital health care infrastructure, created by electronic health records (EHRs), encompasses and leverages digital progress and can transform the way care is delivered and compensated. With EHRs, information is available whenever and wherever it is needed.
“EHRs give providers reliable access to a patient’s complete health information. This comprehensive picture can help providers diagnose patients’ problems sooner.”
EHRs can reduce errors, improve patient safety, and support better patient outcomes because they don’t just contain or transmit information; they “compute” it, for example, cross-referencing prescribed medications, alerting physicians to patient allergies and so on.
The Health Information Technology for Economic and Clinical Health (HITECH) Act, a component of the American Recovery and Reinvestment Act of 2009, represents the nation’s first substantial commitment of federal resources to support the widespread adoption of EHRs. This legislation includes incentives to encourage use of EHRs and other health information technology, based on a concept called “Meaningful Use.”
Meaningful Use requires the use of an EHR as well as a demonstration that it is used to meet objective and measurable requirements. It also includes the standardization of data formats, a requirement that patients are able to easily access and download their digital medical records and images for their own use, expansion of the scope of quality metrics tracking to include specialists and to reflect outcomes, as well as care coordination.
Additional criteria will focus on the sustainability of the program through improvements in quality, safety and efficiency that improve health outcomes.
Kaiser in Colorado Uses Lab Test Data to Improve Cardiac Care
By Robert Michel | From the Volume XVI No. 6 – April 27, 2009 Issue
CEO SUMMARY: Proud of a 73% reduction in mortality among patients with coronary artery disease (CAD) at Kaiser Permanente Colorado, clinical care teams there demonstrate how integrated care and more effective use of laboratory test data can lead to remarkable improvements in pati…
Labs in U.S. and Australia Learn from Each Other
By Robert Michel | From the Volume XIV No. 16 – November 19, 2007 Issue
CEO SUMMARY: Australia just conducted its first summit meeting on laboratory management and a near sell-out crowd showed up to learn the best and latest. For the Americans in the audience, there were several surprises. First, Australia has a highly-competitive laboratory sector, comparabl…
Full Pathology Digitization Is Becoming Feasible
By Robert Michel | From the Volume XIV No. 15 – October 29, 2007 Issue
CEO SUMMARY: Advances in computer hardware, software and support systems such as scanners are bringing the era of full pathology digitization closer to reality. Last week, in San Diego, California, an enthusiastic crowd of several hundred gathered to learn how laboratories, hospitals, and…
CURRENT ISSUE
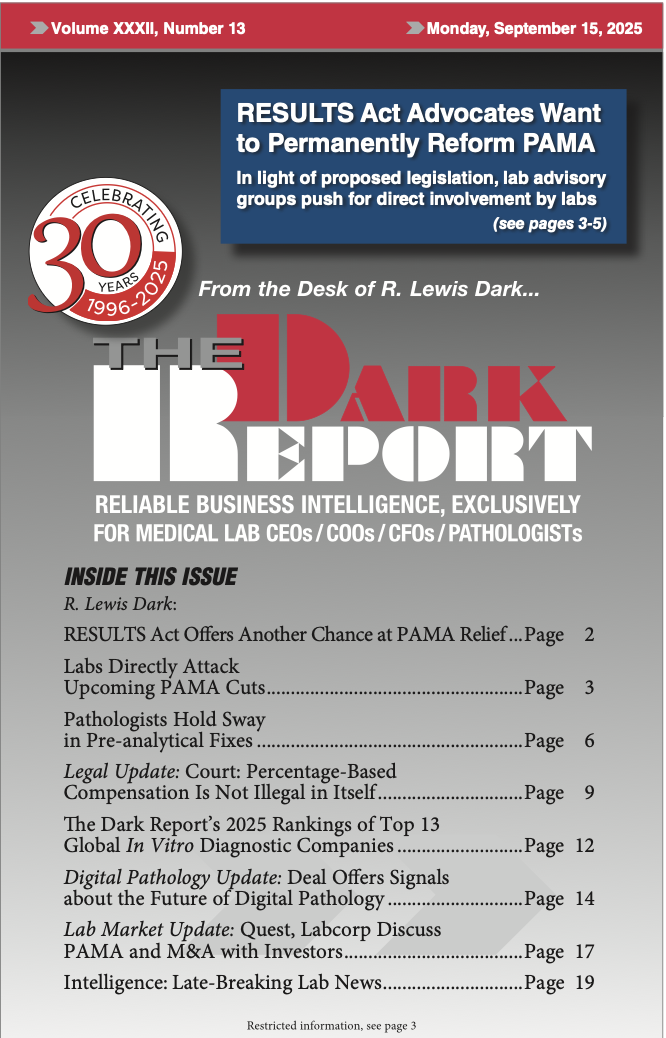
Volume XXXII, No. 13 – September 15, 2025
The Dark Report examines a new bill that would reform PAMA and avoid reimbursement rate cuts scheduled for January 2026. Clinical laboratory leaders are urged to make their voices heard in Congress. Also, an expert describes how labs can fix pre-analytical errors and avoid disaster.
See the full table of contentsHow Much Laboratory Business Intelligence Have You Missed?
Lab leaders rely on THE DARK REPORT for actionable intelligence on important developments in the business of laboratory testing. Maximize the money you make-and the money you keep! Best of all, it is released every three weeks!
Sign up for TDR Insider
Join the Dark Intelligence Group FREE and get TDR Insider FREE!
Never miss a single update on the issues that matter to you and your business.
Topics
- Anatomic Pathology
- Clinical Chemistry
- Clinical Laboratory
- Clinical Laboratory Trends
- Digital Pathology
- Genetic Testing
- In Vitro Diagnostics
- IVD/Lab Informatics
- Lab Intelligence
- Lab Marketplace
- Lab Risk & Compliance
- Laboratory Automation
- Laboratory Billing
- Laboratory Compliance
- Laboratory Equipment
- Laboratory Information Systems
- Laboratory Management
- Lean Six Sigma
- Managed Care Contracts
- Molecular Diagnostics
- Pathology Trends
- People
- Uncategorized

