Managed Care Contracts
Managed care is a health care delivery system organized to manage cost, utilization, and quality. Every healthcare provider must settle on a managed care contract between itself and the payer.
According to Findlaw.com, the contract between a clinical laboratory or other health care professional and a managed care organization (MCO) such as a provider-sponsored network, integrated delivery system, health maintenance organization, or other health care plan, is the fundamental document which frames, defines and governs their relationship. Contractual provisions can affect payment, office organization, practices and procedures, and confidential records as well as clinical decision-making.
Findlaw states, “A good managed care contract, like any other form of business agreement, is clear, consistent, comprehensive, and concise. It will conform to both the intent of the parties, setting out their respective rights and responsibilities, and the requirements of state and federal law.”
For example, Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations (MCOs) that accept a set per member per month (capitation) payment for these services.
Depending on the market share of the health plan and the services offered by the healthcare provider, the negotiability of the contract will vary. Well-established managed care plans that have a large market share typical use form contracts. Newer managed care plans that have little market share and want broad provider participation are generally more willing to negotiate terms.
The Patient Protection and Affordable Care Act and the move toward accountable care has put a much greater emphasis on quality measures than in previous years.
Healthcare providers must prove in contract negotiations how well they manage quality and cost; such proof is usually provided with a comprehensive set of quality measures reported directly from the electronic health record (EHR). This can be straightforward for a single practice using the basic reporting functionality of its EHR, a more complex managed care plan might require features that an EHR vendor doesn’t offer.
Layoffs at Major Health Plans Slow Processing of Lab Claims
By Virchow | From the Volume XXXII, No. 3 – February 17, 2025 Issue
…
Why Payers Bristle as Labs Submit Inpatient Fees for Outreach Tests
By Virchow | From the Volume XXXII, No. 3 – February 17, 2025 Issue
EDITOR’S NOTE: Our column, Virchow, is written…
How Certain Labs Can Crack into Health Plans’ Closed Networks
By Virchow | From the Volume XXXII, No. 3 – February 17, 2025 Issue
EDITOR’S NOTE: Our column, Virchow, is written by anonymous insiders working within the managed…
Gaining Network Access with Payers Is Often about Geography
By Virchow | From the Volume XXXII, No. 3 – February 17, 2025 Issue
EDITOR’S NOTE: Our column, Virchow, is written by anonymous insiders working within the managed…
How Private Payers Audit Labs for Possible Claims Fraud
By Virchow | From the Volume XXXII, No. 3 – February 17, 2025 Issue
EDITOR’S NOT…
Private Health Insurers Are Aware of Problems with CPT Code 81408
By Virchow | From the Volume XXXII, No. 3 – February 17, 2025 Issue
EDITOR’S NO…
UHC Will Delay Enforcement of Z-codes for Genetic Test Claims
By Scott Wallask | From the Volume XXXII, No. 3 – February 17, 2025 Issue
IN THE LATEST BACKPEDAL ON ITS NEW POLICY, UNITEDHEALTHCARE (UHC) appears to have dropped its requirement for genetic testing laboratories to use Z-codes for claims under commercial health plans—for now. Earlie…
Smaller Labs Must Verify Z-code Arrangement with Lab Companies
By Virchow | From the Volume XXXII, No. 3 – February 17, 2025 Issue
EDITOR’S NO…
With Z-codes, Will Other Payers Follow UnitedHealthcare’s Lead?
By Virchow | From the Volume XXXII, No. 3 – February 17, 2025 Issue
EDITOR’S NOT…
Technical Assessment Challenges for Z-Code Applications
By Scott Wallask | From the Volume XXXII, No. 3 – February 17, 2025 Issue
CEO SUMMARY: Effective on Aug. 1, UnitedHealthcare will require Z-code submissions for many genetic tests. During a recent webinar, experts tackled a topic that may prove troublesome for labs seeking Z-codes: technical assessments. Key advice is to provide specific data about clin…
CURRENT ISSUE
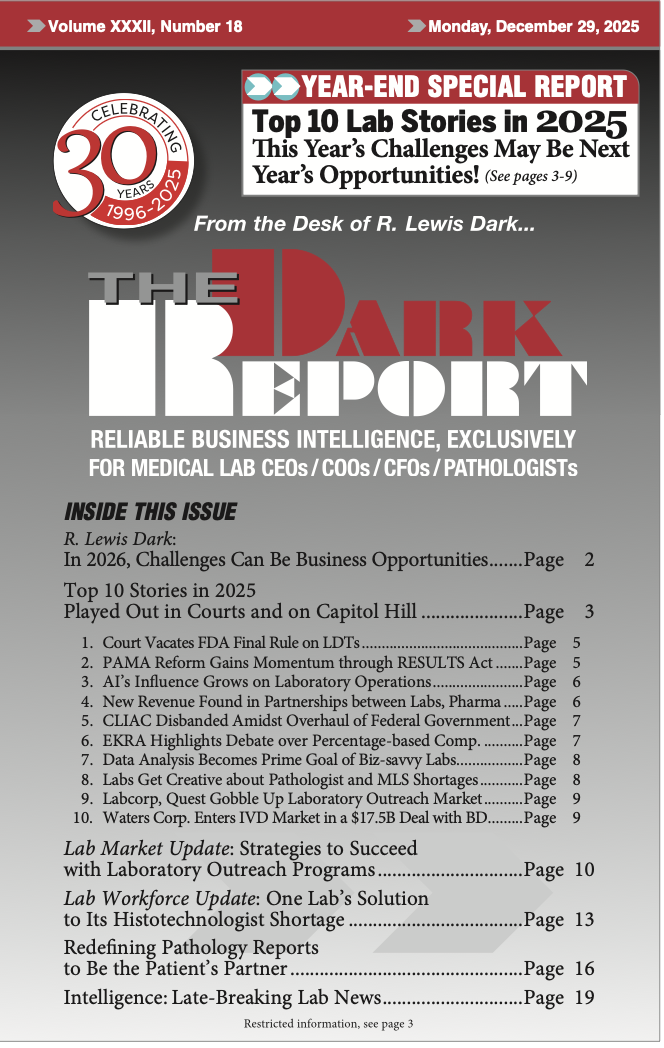
Volume XXXII, No. 18 – December 29, 2025
The Dark Report reviews its top 10 stories from 2025, from the vacating of the FDA’s LDT rule to the merger of Waters and Becton Dickinson’s biosciences and diagnostics units. Also, a lab outlines its solution to a shortage of histotechnologists, and another story shows how pathologists can become patients’ partners.
See the full table of contentsHow Much Laboratory Business Intelligence Have You Missed?
Lab leaders rely on THE DARK REPORT for actionable intelligence on important developments in the business of laboratory testing. Maximize the money you make-and the money you keep! Best of all, it is released every three weeks!
Sign up for TDR Insider
Join the Dark Intelligence Group FREE and get TDR Insider FREE!
Never miss a single update on the issues that matter to you and your business.
Topics
- Anatomic Pathology
- Clinical Chemistry
- Clinical Laboratory
- Clinical Laboratory Trends
- Digital Pathology
- Genetic Testing
- In Vitro Diagnostics
- IVD/Lab Informatics
- Lab Intelligence
- Lab Marketplace
- Lab Risk & Compliance
- Laboratory Automation
- Laboratory Billing
- Laboratory Compliance
- Laboratory Equipment
- Laboratory Information Systems
- Laboratory Management
- Lean Six Sigma
- Managed Care Contracts
- Molecular Diagnostics
- Pathology Trends
- People
- Uncategorized

