CEO SUMMARY: Experts point out that widely publicized episodes of lab testing deficiencies in several provinces are signs that chronic underfunding of lab testing services is a key factor in these failures. To restore public confidence in breast cancer testing, the Canadian Association of Pathologists is developing a voluntary proficiency testing system for hospital labs …
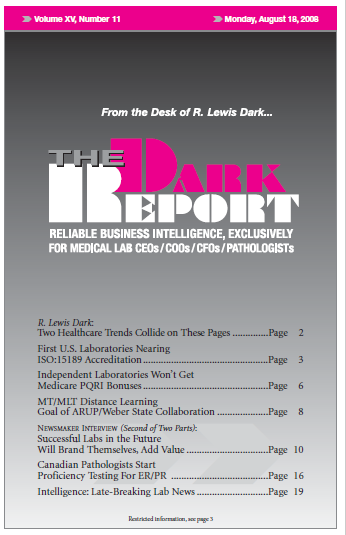
Canadian Pathologists Start PT Testing for ER/PR Read More »
To access this post, you must purchase The Dark Report.