MANAGED CARE PLANS are taking aggressive steps to keep clinical lab testing within their preferred networks. In particular, Aetna, Inc., is earning a reputation as one of the toughest insurers in this regard. Most recently, in a letter sent to at least one network physician, Aetna warned the physician that, if the doctor continued to …
Aetna Threatens to Expel Docs for Out-of-Network Lab Referrals Read More »
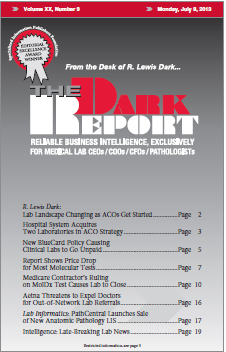
To access this post, you must purchase The Dark Report.