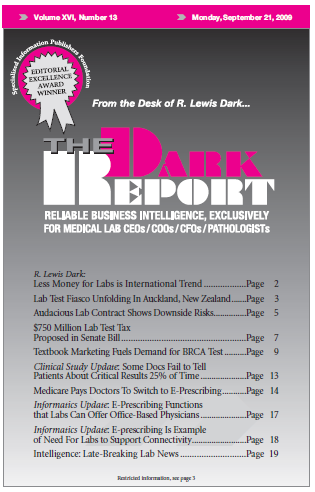
CEO SUMMARY: It’s a major step on the road to integration of healthcare informatics. During the next few years, the Medicare program is offering financial incentives to encourage office-based physicians to adopt e-prescribing. This is a positive development for local laboratories and hospital lab outreach programs. Early-adopter labs are already taking steps to enable e-prescribing …
Medicare Pays Doctors To Switch to E-Prescribing Read More »
To access this post, you must purchase The Dark Report.