CEO SUMMARY: In court papers, Cigna alleged that HDL misrepresented patients’ responsibilities by promising not to collect co-payments, co-insurance, or deductibles. Also, HDL promised not to seek reimbursement from patients for any portion of its bills that the health insurer did not cover, the court documents show. HDL misleadingly billed the health insurer at exorbitant …
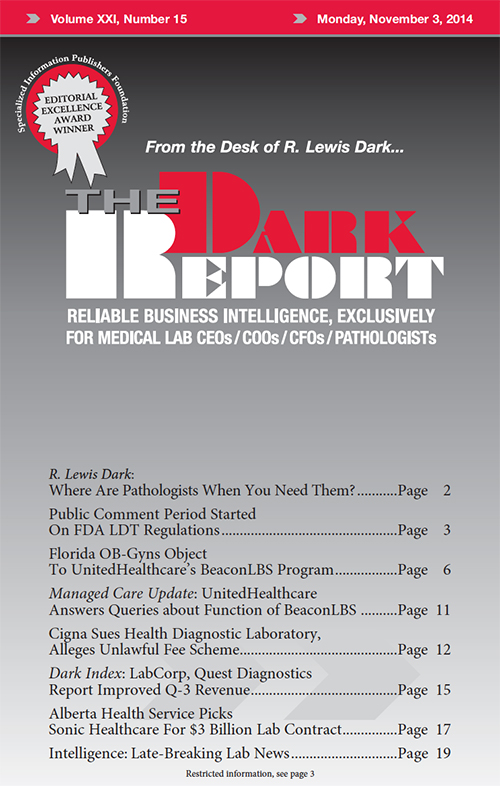
Cigna Sues HDL, Alleges Unlawful Fee Scheme Read More »
To access this post, you must purchase The Dark Report.