CEO Summary: Pre-authorization of expensive genetic and molecular tests is fast-becoming a priority for most of the nation’s health insurers. For clinical labs and pathology groups that don’t respond, this trend is a threat. On the other hand, because payers need all the skills and knowledge that labs possess to intelligently manage utilization of molecular …
Payers Move to Pre-Authorize Expensive Genetic Tests Read More »
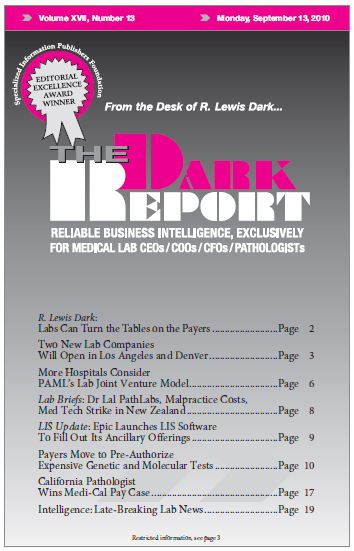
To access this post, you must purchase The Dark Report.