OVERWHELMED WITH REQUESTS TO PAY for new genetic tests, health insurers, particularly smaller and regional insurers, find it easier to simply deny payment for such tests.
To access this post, you must purchase The Dark Report.
OVERWHELMED WITH REQUESTS TO PAY for new genetic tests, health insurers, particularly smaller and regional insurers, find it easier to simply deny payment for such tests.
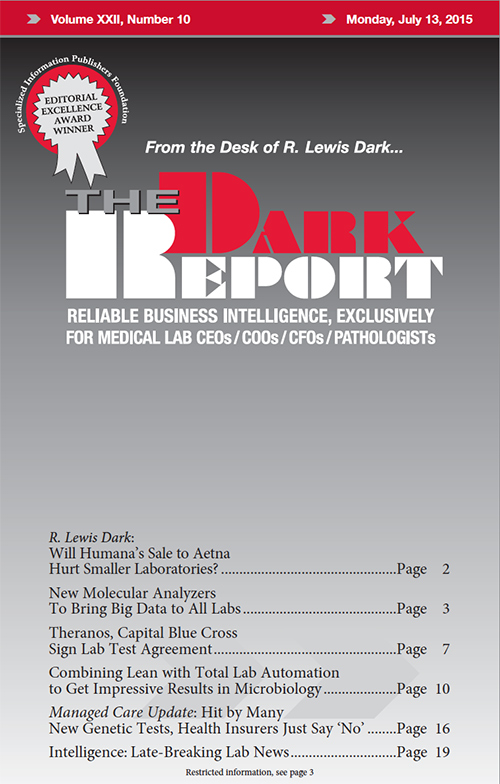
Volume XXII No. 10 – July 13, 2015
COMMENTARY & OPINION BY R. LEWIS DARK
ARTICLES
INTELLIGENCE
The Dark Report • 21806 Briarcliff Dr • Spicewood, TX 78669
Phone: 512-264-7103 • Toll Free Number: 800-560-6363
Email: info@darkreport.com
© 2024 The Dark Report. All rights reserved.