APRIL 15 IS THE DATE when UnitedHealthcare will begin denying laboratory claims in Florida that do not meet the requirements of its unpopular laboratory benefit management program.
To access this post, you must purchase The Dark Report.
APRIL 15 IS THE DATE when UnitedHealthcare will begin denying laboratory claims in Florida that do not meet the requirements of its unpopular laboratory benefit management program.
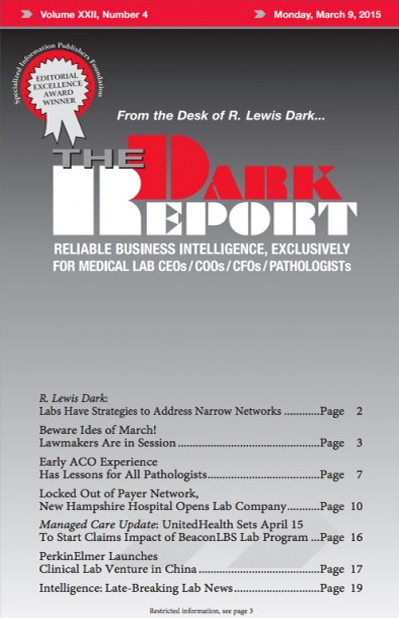
Volume XXII No. 4 – March 9, 2015
COMMENTARY & OPINION BY R. LEWIS DARK
ARTICLES
INTELLIGENCE
The Dark Report • 21806 Briarcliff Dr • Spicewood, TX 78669
Phone: 512-264-7103 • Toll Free Number: 800-560-6363
Email: info@darkreport.com
© 2024 The Dark Report. All rights reserved.