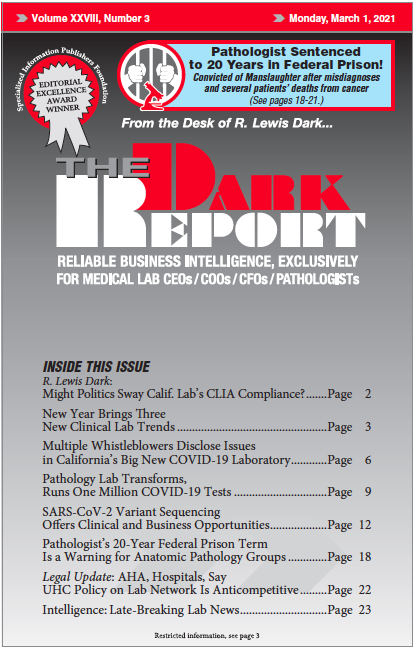
CEO SUMMARY: In January, a former VA pathologist was sentenced to 20 years in federal prison following his conviction on charges of involuntary manslaughter and mail fraud. The facts in this case show why leaders of clinical labs and pathology groups need to be aware of individuals who are impaired on the job due to …
Pathologist’s Prison Term Is a Warning for AP Groups Read More »
To access this post, you must purchase The Dark Report.