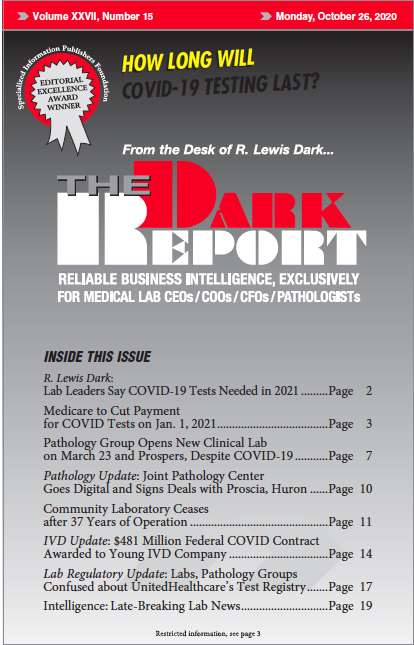
This is an excerpt of a 1,9842-word article in the October 26, 2020 issue of THE DARK REPORT (TDR). The full article is available to members of The Dark Intelligence Group. CEO SUMMARY: Starting Jan. 1, CMS will lower the Medicare COVID test payment to $75 when labs with “high-throughput systems” report a COVID-19 test result …
Medicare COVID Test Payments to Be Cut Starting Jan. 1 Read More »
To access this post, you must purchase The Dark Report.