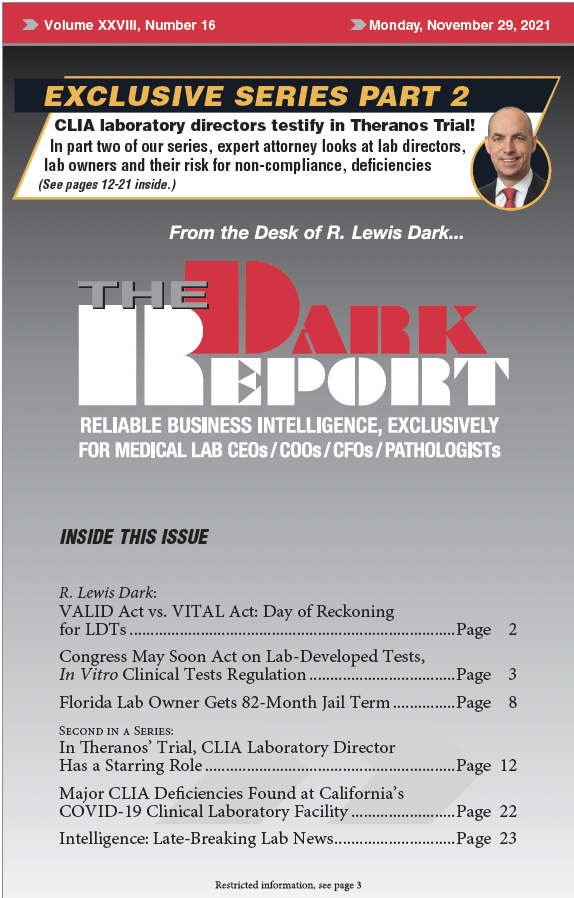
This is an excerpt of a 2,017-word article in the November 29, 2021 issue of THE DARK REPORT (TDR). The full article is available to members of The Dark Intelligence Group. CEO SUMMARY: Congress is gearing up for a debate on laboratory-developed tests (LDT) regulation and that of other in vitro clinical tests (IVCTs). The VALID […]
To access this post, you must purchase The Dark Report.