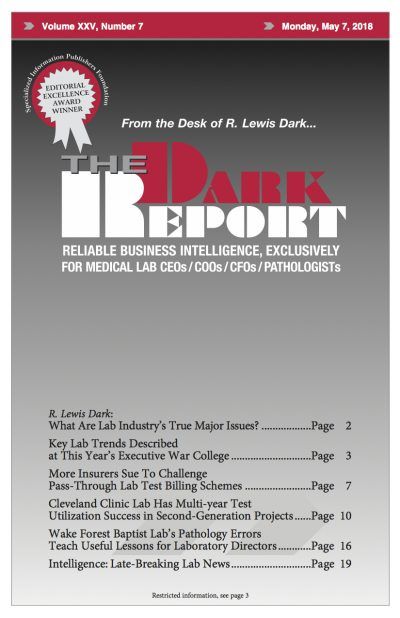
This is an excerpt from a 2,920-word article in the May 7, 2018 issue of THE DARK REPORT. The complete article is available for a limited time to all readers, and available at all times to paid members of the Dark Intelligence Group. CEO SUMMARY: In an insightful report, THE DARK REPORT shows how one …
Cleveland Clinic Lab dramatically reduces doctors ordering unnecessary tests Read More »
To access this post, you must purchase The Dark Report.