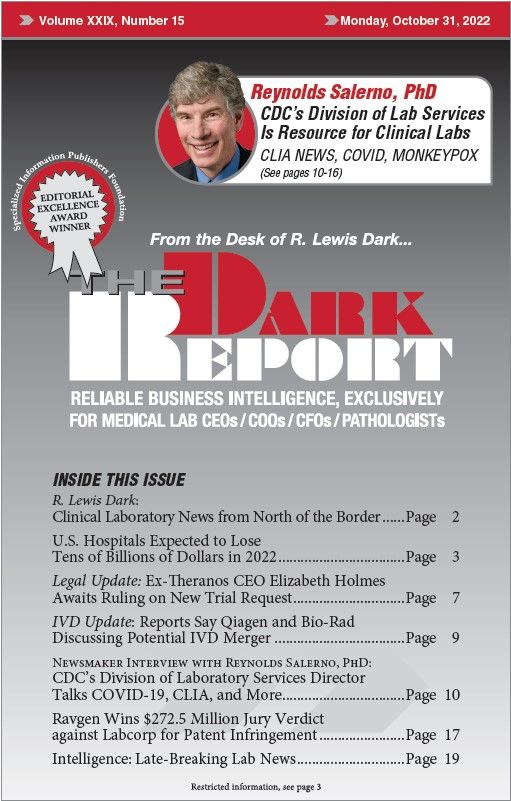
CEO SUMMARY: In this exclusive interview, Reynolds Salerno, PhD, the Director of the Division of Laboratory Systems at the CDC, offers insightful comments about the federal agency’s response to the SARS-CoV-2 pandemic, what went right during public health efforts, and lessons that were learned. He also discusses how labs have dealt with the recent monkeypox …
To access this post, you must purchase The Dark Report.