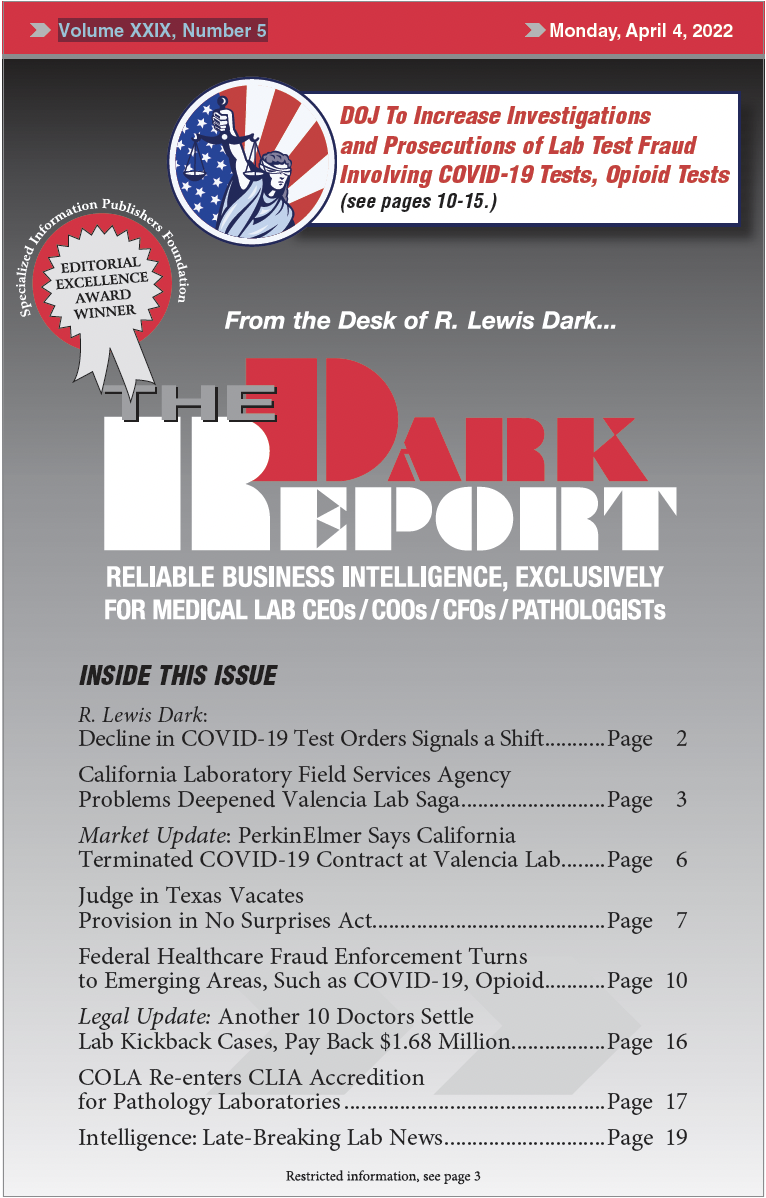
CEO SUMMARY: Healthcare compliance attorneys say the Department of Justice (DOJ) is turning its focus to fraudulent activity related to COVID-19 testing. But that’s not the only area attracting greater scrutiny by the DOJ. Fraud stemming from opioid treatment has snared clinical laboratory companies that ordered medically-unnecessary diagnostic tests. Further, prosecutors have been ordered to …
Federal Healthcare Fraud Enforcement Turns to Emerging Areas Read More »
To access this post, you must purchase The Dark Report.