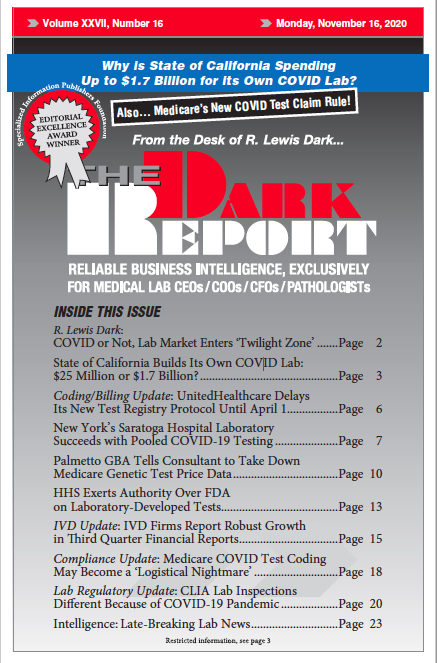
This is an excerpt of a 1,552-word article in the November 16, 2020 issue of THE DARK REPORT (TDR). The full article is available to members of The Dark Intelligence Group. CEO SUMMARY: Pooled COVID testing helps the clinical lab staff at the hospital in Saratoga Springs, N.Y., do more COVID-19 tests when supplies might …
Pooled COVID Testing a Success for New York Hospital Lab Read More »
To access this post, you must purchase The Dark Report.