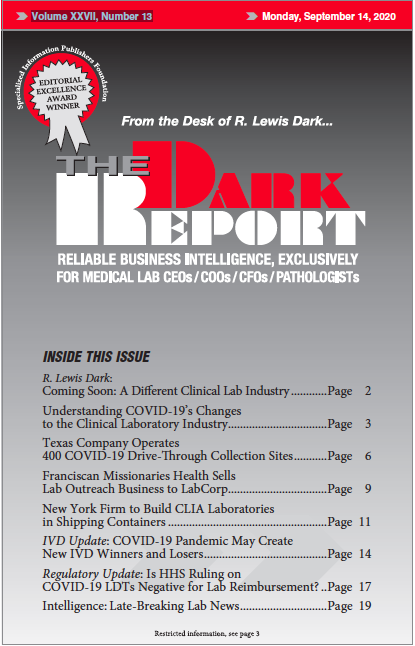
This is an excerpt of a 1,028-word article in the September 14, 2020 issue of THE DARK REPORT (TDR). The full article is available to members of The Dark Intelligence Group. WHILE SOME LABS CELEBRATE THE PERCEIVED FLEXIBILITY that comes from not having to get an emergency use authorization (EUA) for COVID-19 laboratory-developed tests (LDTs), there is a potential […]
To access this post, you must purchase The Dark Report.