CEO SUMMARY: In the 1990s, many hospitals implemented decentralized phlebotomy arrangements as a way to save costs. Now, a decade later, centralized phlebotomy, managed by the laboratory, is making a comeback. Motivation for this unfolding trend is the need for hospitals to improve patient safety and increase patient satisfaction. Because most patients are uncomfortable with venipuncture, …
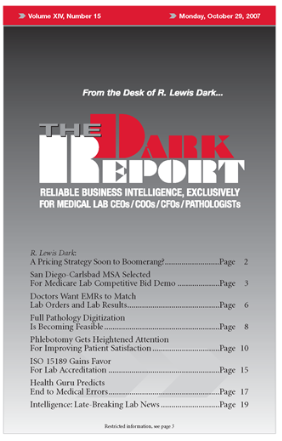
Phlebotomy Gets Heightened Attention For Patient Satisfaction Read More »
To access this post, you must purchase The Dark Report.