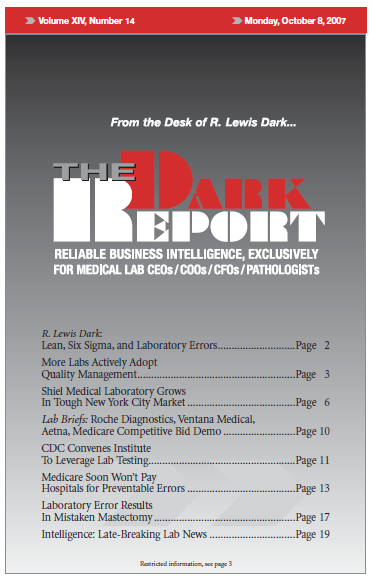
CEO SUMMARY: CMS issued new rules, effective in October 2008, that it will no longer pay the extra cost of treating patients after preventable errors, infections, or injuries that occur in hospitals. It continues Medicare’s transformation from a “passive payer simply processing claims” to an “active purchaser with a stake in quality and efficiency.” Many …
Medicare Soon Won’t Pay Hospitals for Errors Read More »
To access this post, you must purchase The Dark Report.