MEDICARE MANAGED CARE PLANS are poised to double in size. This can be both a threat and an opportunity for regional laboratories. The Center for Medicare and Medicaid Services (CMS) recently reported that it had received 141 applications for new local Medicare Advantage plans for 2005. The applications included 55 HMOs, 73 PPOs, and 13 …
Medicare Managed Care Is Poised to Double in Size Read More »
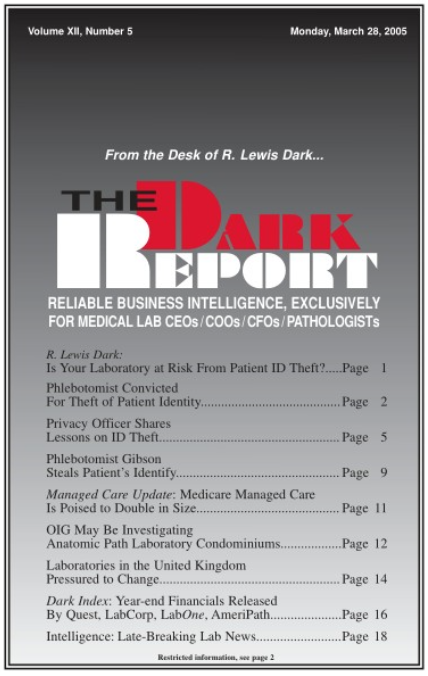
To access this post, you must purchase The Dark Report.