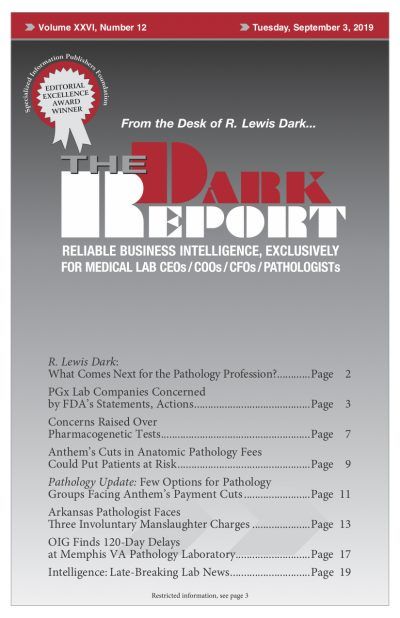
CEO SUMMARY: Last year, Veterans Administration officials received an anonymous complaint about delays in laboratory specimen processing and results at the Memphis VA Medical Center may have harmed patients and led to a patient death. Following an investigation, the VA’s Office of Inspector General issued a report last month. It determined that a staff shortage …
OIG Finds 120-Day Delays at Memphis VA Path Lab Read More »
To access this post, you must purchase The Dark Report.