CEO SUMMARY: By issuing a multi-count criminal indictment against three former UroCor executives, one federal attorney is creating new legal precedents for the laboratory industry. The criminal charges accuse UroCor of inducing physicians through such gambits as deeply-discounted pricing and “free testing” when not a contracted network laboratory. Labs should review compliance with these types …
UroCor’s Sales Tactics Violated Medicare Laws Read More »
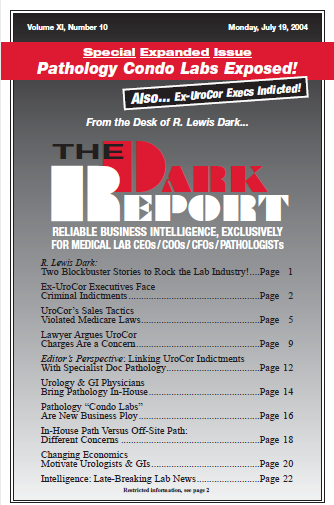
To access this post, you must purchase The Dark Report.