CEO SUMMARY: Forty years ago, pathologists in hospital and academic labs worked closely with treating physicians to produce laboratory-developed tests for discrete clinical cases. Seeing that, the FDA decided not to regulate those tests, an FDA official said. Over time, however, use of LDTs became a serious concern when labs developing LDTs were no longer involved …
FDA Official Makes Case In Favor of LDT Guidance Read More »
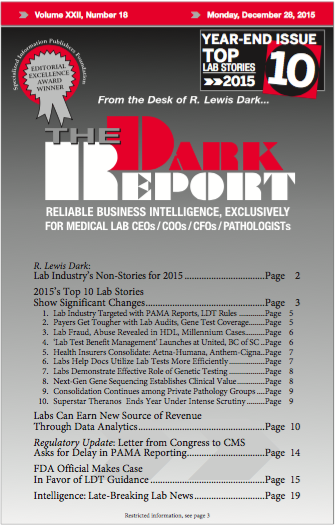
To access this post, you must purchase The Dark Report.