FLORIDA IS ONCE AGAIN GROUND ZERO for a major case of lab testing fraud. UnitedHealthcare has filed suit against five toxicology laboratory companies, three general partners in those companies, eight urinalysis referral sources, and other entities, claiming the defendants defrauded the health insurer of more than $50 million. Filed last month in U.S. District Court …
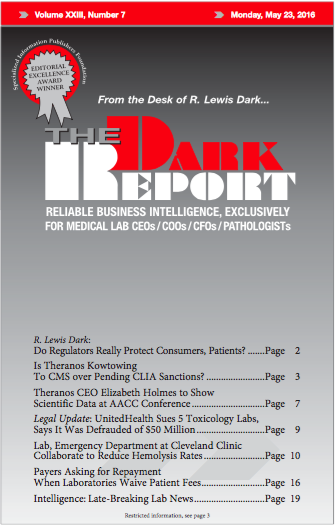
UnitedHealth Sues 5 Tox Labs, Says It Was Defrauded of $50M Read More »
To access this post, you must purchase The Dark Report.