CEO SUMMARY: Members of Joint Venture Hospital Laboratories in Michigan anticipate that the 2018 Clinical Laboratory Fee Schedule rates being implemented under PAMA will lower payment from Medicare to less than the cost of running tests, especially for rural and critical access hospitals. CMS established the 2018 CLFS under the Patient Access to Medicare Act …
Lab Executives Declare Concerns about Fee Cuts Read More »
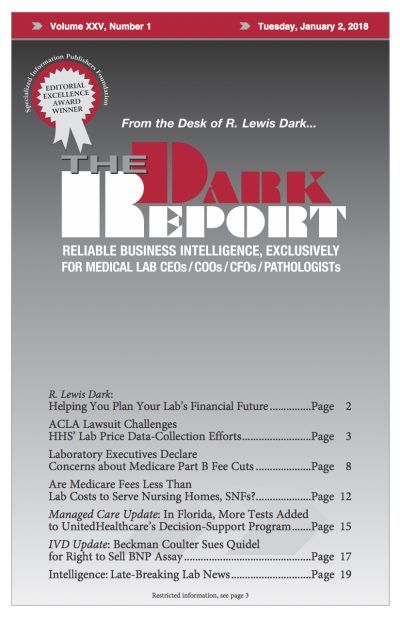
To access this post, you must purchase The Dark Report.