CEO SUMMARY: Each year, over 100 million new prescriptions are written for two classes of drugs with metabolic pathways affected by genetic variations in cytochrome P450. There are strong clinical arguments in favor of testing individuals for these genetic mutations to determine whether they are no, slow, or ultra-fast metabolizers of these drugs, before writing …
CYP450 Plays Major Role In Drug Metabolization Read More »
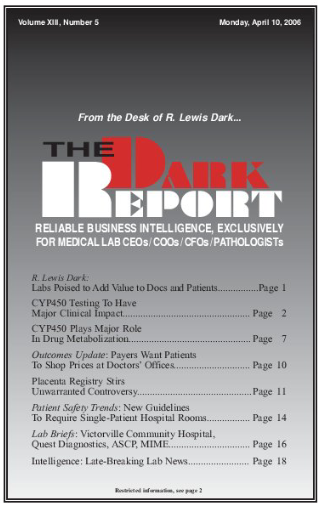
To access this post, you must purchase The Dark Report.