CEO SUMMARY: On the surface, the “exposé” published by The Oregonian newspaper on February 12 seemed designed to sensationalize an effort by local obstetricians, hospitals, and pathologists to do a better job of evaluating placentas taken from patients who had experienced a difficult birth as an arrangement intended to provide a defense in malpractice cases. …
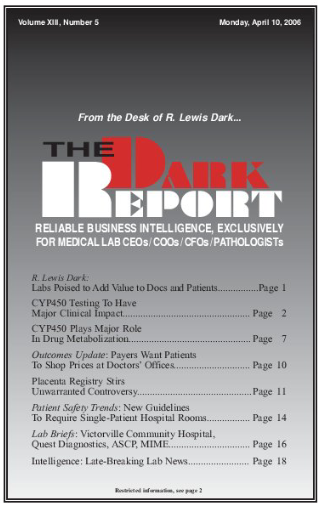
Placenta Registry Stirs Unwarranted Controversy Read More »
To access this post, you must purchase The Dark Report.