ONE CONSEQUENCE of the terrorist attacks on September 11 is that proposed reforms to Medicare lab reimbursement policies have assumed a lesser priority with the current Congress. Despite that fact, Congress must still address the day-to-day requirements of managing government functions. Thus, there is still activity under way to develop and pass bills affecting funding …
Certain Medicare Lab Reforms May Make It Through Congress Read More »
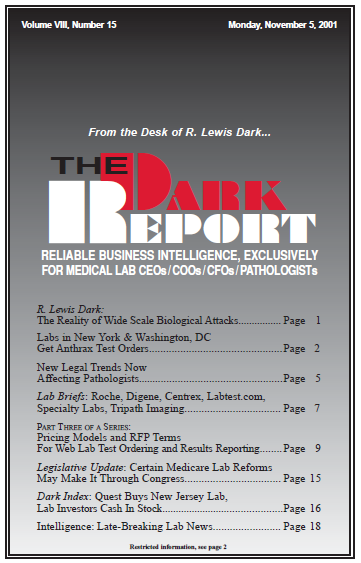
To access this post, you must purchase The Dark Report.