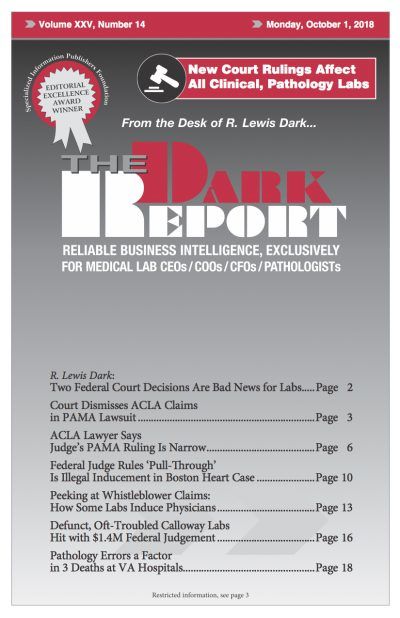
This is an excerpt from a 2,400-word article in the October 1, 2018 issue of THE DARK REPORT. The complete article is available at all times to paid members of the Dark Intelligence Group, and non-members may access one premium article per month. CEO SUMMARY: Many lab professionals are disappointed at the news that there …
No relief in sight for 2018 Clinical Laboratory Fee Schedule, but critical issues remain Read More »
To access this post, you must purchase The Dark Report.