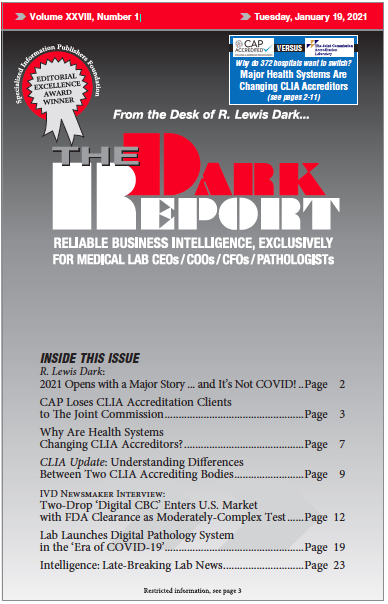
This is an excerpt of a 1,790-word article in the January 19, 2021 issue of THE DARK REPORT (TDR). The full article is available to members of The Dark Intelligence Group. CEO SUMMARY: Over the past 18 months, several prominent national health systems decided to shift their CLIA laboratory accreditation services away from the College …
CAP Loses CLIA Accreditation Clients to Joint Commission Read More »
To access this post, you must purchase The Dark Report.